
Implantable Sensors are smaller than a grain of rice and made up of hydrogel scaffold that’s flexible as a contact lens.
A Medical procedure that separates patients into different group Personalized medicine is one step closer for consumers, by creating an implantable sensor that gives warning before health problems develop in a human body. Scientists are developing and have begun marketing their first device in Europe and hopes for getting approval over this in the U.S.
“Other implantable sensors currently on the market have a significant drawback,” Natalie A. Wisniewski, Ph.D., says. “They often provoke a ‘foreign body’ immune response that coats the sensor with inflammatory cells or scar tissue.” That coating can wall off the device from capillaries and prevent it from sensing chemical changes accurately, so it stops working after a few weeks or months.
“The researchers also made sure their sensor lacks any flat surfaces, which are a dead giveaway to cells that an object isn’t natural”, says Wisniewski, who is at Profusa Inc. He also announced that the first sensor implanted in human volunteers are still functioning after more than 4yrs. Therefore, cells and capillaries grow into the sensor’s structure without enabling the undesirable immune response.
The hydrogel is the formulation based on poly (2-hydroxyethyl methacrylate). The same polymer which is used in making soft contact lenses. Researchers covered the hydrogel scaffold with the dye molecules that respond to the concentration of an analyte like oxygen, co2, glucose, or lactate, in the blood.
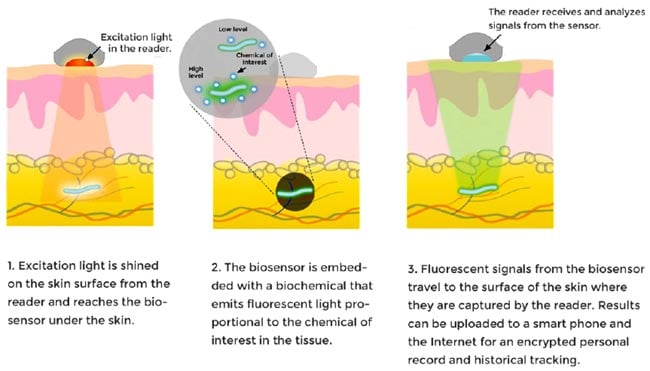
A small detector is patched against the skin, which shines near-infrared light through the skin. It causes the dye molecules to fluoresce more or less brightly according to the concentration of the analyte. That fluorescent light is not visible to human eye, it can only be seen by a detector which wirelessly sends the measurement of change in brightness (as the analyte concentration fluctuates over time) to the computer or mobile phone to record the change. It has been shown to report tissue oxygen levels in patients under treatment for peripheral artery disease, which affects millions of people worldwide. This disease affects the oxygen level which causes amputation. So, to prevent amputation this device is used. It helps by informing the physician about the decrement in the oxygen levels in a patients limbs.
The modification of this idea is to track multiple body chemistries at the same time. “The sensors would provide a continuous record of your analytes relative to your personal baseline,” Wisniewski explains. “Then if something goes off-kilter, it’s flagged early, before you feel symptoms, so you can get to the doctor in time for treatment.”
Wisniewski says that “the military is also interested in these devices, and has provided support since the company’s inception. They envision the use of the sensor is effective for the soldiers and the athletes. This research is supported by various Government bodies National Institutes of Health (NIH) and the Defense Advanced Research Projects Agency (DARPA).

